A VOC is the hallmark acute complication for persons with SCD and manifests as acute severe pain. Although VOCs are typically associated with excruciating pain of sudden onset, some people experience gradual onset of a voc. Nearly all individuals affected by SCD will experience a voc during their lifetime. The first voc may occur as early as 6 months of age, often presenting as dactylitis, but thereafter VOCs occur with variable frequency. VOCs and their accompanying pain most commonly occur in the extremities, chest, and back. When they occur in other sites, they can be confused with, or can be the prodromal stage of, other acute complications (e.g., head (stroke), flank (papillary necrosis), and abdomen (hepatic or splenic sequestration, constipation from opioid toxicity, or another hepatobiliary complication)). The etiology of the pain must be determined in order to rule out potential causes of pain other than an uncomplicated VOC, such as ACS, pneumonia, or other abdominal complications. VOC can still occur in the presence of other complications.
There are no tests to rule in or to rule out a VOC; there are only tests that potentially rule out other causes of pain_ Persons with the genotypes HbSS or HbS 0-thalassemia are likely to experience more frequent VOCs. Persons with HbAS (commonly referred to as sickle cell trait) do not experience typical VOCs. Individuals with more than three hospitalizations for a VOC in a year are at an increased risk of early death.
Pain management must be guided by patient report of pain severity_ No biomarkers or imaging studies can validate pain or assess its severity. The primary management of a VOC is analgesic treatment, typically with opioids. No empirical data exist to indicate that rapid analgesic administration results in better outcomes.
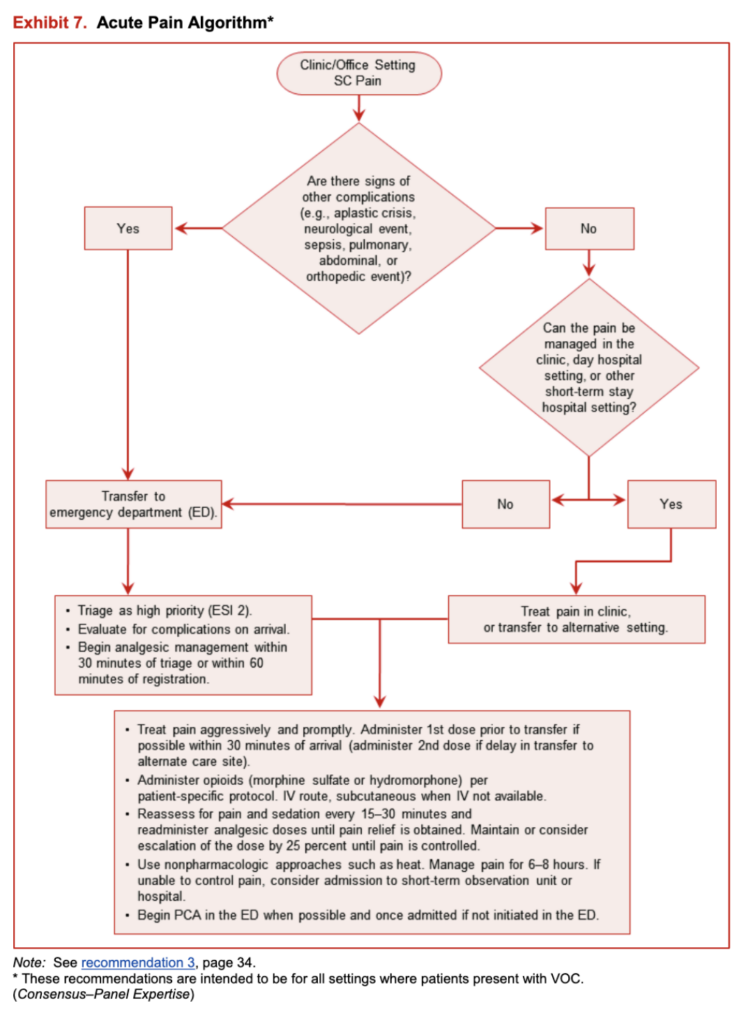
However, as patients with VOC present with severe pain and are at risk for other complications, best practice suggests that rapid triage, placement, and administration of analgesics should be encouraged. The Emergency Severity Index (ESI) Version 4 triage system, which is used by more than half of emergency departments in the United States, suggests that persons with SCD be triaged as ESI level 2, a very high priority, and rapid placement be facilitated.
Many specific recommendations for acute VOC management are included in this section that address treatment beyond what is listed in the Key Question (below). The expert panel felt it was important to include current practices that have not yet been validated by evidence, but are currently being used. When made, these recommendations are clearly identified as “Consensus-Panel Expertise.” A recommendation is included to guide providers in managing persons who take both long- and short-acting opioids to manage pain at home.
There are no empirical data to guide whether or not to continue long-acting opioids when ordering continuous opioids via patient-controlled analgesia (PCA). The decision to continue long-acting oral opioids should be made on an individual basis_ In most circumstances, it is advisable to continue oral long-acting opioids including methadone therapy even when ordering continuous opioids via PCA to ensure adequate pain relief while avoiding a break in coverage and preventing withdrawal. Finally, hydration and nonpharmacological therapy are also very important as is concurrent treatment of itching caused by histamine release.
Summary of the Evidence
Thirty-two ReTs with more than 1,800 people of all ages, 34 observational studies, and 30 case reports were considered eligible. Because many of these studies evaluated pharmacologic agents that did not decrease pain or significantly reduce length of hospital stay (e.g., poloxamer 188, fluosol, vasodilators, methylprednisone, oxygen, urea, and other agents), and which are not approved by the U.S. Food and Drug Administration (e.g., inhaled nitrous oxide, transfusion, etc.), recommendations regarding these agents were not made. One study evaluated the effectiveness of meperidine versus placebo or other opioids and found meperidine more effective than placebo in reducing pain. However, due to the neurotoxicity associated with meperidine, the panel did not make recommendations for its use. Evidence from several ReTs and observational studies supports the use of opioid therapy in treating voes. Indirect, high-quality evidence from populations without sen also supports the use of opioids in treating VOCs. A recent report from the American Pain Society (APS) suggests opioids are not effective in treating chronic non-cancer pain.154 It is important to understand that an acute VOC is considered acute, not chronic pain, and opioids are indicated and should be used to treat pain. Evidence from ReTs and observational studies supporting the use of nonsteroidal anti-inflammatory drugs (NSAIDs) was conflicting, but overall, the evidence supports their efficacy in reducing pain and decreasing length of hospital stay. Several RCTs and observational studies support the use of around-the-clock dosing of analgesics versus intermittent analgesic administration in treating VOCs.
The largest study on this topic, a prospective observational study in Saudi Arabia, included 1,154 people and examined the effect of a pain management protocol. The study found that around-the-clock analgesic infusions for the first 24 hours after admission were more effective for managing voes than “on demand” or patient-requested infusions of analgesics. People treated with around-the-clock analgesics achieved a higher discharge rate within 72 hours of admission (83 percent), compared with people who received intermittent (per patient request) analgesics (Tl percent). Other observational studies supported these findings and also suggested a more rapid resolution of VOCs and a strong patient preference for around-the-clock analgesic infusions. The evidence base was insufficient to make specific analgesic dosing recommendations or recommendations for several nonpharmacologic approaches (including oxygen, inhaled nitrous oxide, electrical nerve stimulation, acupuncture, biofeedback, and a day hospital program). In general, the quality of the available evidence was moderate to low.
In addition, the panel and the methodology team appraised the quality of the APS’s guidelines for the management of sen-related pain and found them to be acceptable. As shown in the “Consensus-Adapted” recommendations below, the panel adapted selected recommendations from the APS guidelines for treatment of SCD pain. Additional recommendations are based upon the experience of the expert panel and are categorized as “Consensus-Panel Expertise.”
Recommendations
The recommendations labeled “consensus” in this section were based on recommendations developed by the APS or on panel expertise. The remaining recommendations are based on the evidence review conducted by the methodology team. These recommendations are intended to be for all settings where patients present with VOC.
In adults and children with SCD and pain,
When indicated, initiate diagnostic evaluation of causes of pain other than a VOC while beginning to treat pain. (Consensus-Adapted)
In adults and children with SCD and a voc,
Determine characteristics, associated symptoms, location, and intensity of pain based on patient self-reported observation. If the VOC pain is atypical, investigate other possible etiologies of pain.
(Consensus-Adapted)
Rapidly assess the patient’s recent analgesic use (opioid and nonopioid). (ConsensurAdapted)
Rapidly Initiate analgesic therapy within 30 minutes of triage or within 60 minutes of registration.
(Consensus-Panel Expertise)
Base analgesic selection on pain assessment, associated symptoms, outpatient analgesic use, patient knowledge of effective agents and doses,and past experience with side effects. (Consensus-Adapted)
In adults and children with SCD and a VOC,
Use an individualized prescribing and monitoring protocol (written by the patient’s SCD provider) or an SCD specific protocol whenever possible(see exhibit 7 on page 36) to promote rapid, effective,and safe analgesic management and resolution of the voe. (Consensus-Panel Expertise)
In adults and children with SCD and a VOC associated with mild to moderate pain who report relief withNSAIDS in the absence of contraindications to the use of NSAIDS, continue treatment with NSAIDS.
(Moderate Recommendation, Low-Quality Evidence)
In adults and children with SCD and a VOC associated with severe pain, rapidly initiate treatment with parenteral opioids. (Strong Recommendation, High-Quality Evidence)
In adults and children with SCD and a VOC associated with severe pain, Calculate the parenteral (IV or subcutaneous) opioid dose based on total daily short-acting opioid dose currently being taken at home to manage the voe. (Consensus-Panel Expertise)
Administerparenteral opioids using the subcutaneous route when intravenous access is difficult.
(Consensus-Panel Expertise)
Reassess pain and re-administer opioids if necessary for continued severe pain every 15-30 minutes until pain is under control per patient report. (Consensus-Adapted)
Maintainor consider escalation of the dose by 25 percent until pain is controlled. (Consensus-Panel Expertise)
Reassess after each dose for pain relief and side effects. (Consensus-Panel Expertise)
Initiate around-the-clock opioid administration by patient-controlled analgesia(PCA) or frequently scheduled doses versus “as requested” (PRN) administration. (Moderate Recommendation, Low-Quality Evidence)
If ordering around-the-clock, continuous infusion of opioids via the PCA, carefully consider whether there is a need to withhold long-acting oral opioids to prevent over-sedation. (Consensus-Panel Expertise)
If demand dosing only is ordered via the PCA, continue use of long-acting oral opioids.
(Consensus-Panel Expertise)
At discharge, evaluate inpatient analgesic requirements, wean parenteral opioids prior to conversion to oral opioids, and adjust home dose of long- and short-acting opioid prescriptions to prevent opioid withdrawal after discharge. (Consensus-Panel Expertise)
In adults and children with SCD and a VOC, do not use meperidine unless it is the only effective opioid for an individual patient. (Consensus-Adapted)
In adults and children with a VOC, administer oral NSAIDS as an adjuvant analgesic in the absence of contraindications. (Consensus-Adapted)
In adults and children with a VOC who require antihistamines for itching secondary to opioid administration,prescribe agents orally, and do not re-administer with each dose of opioid in the acute VOC management phase. Re-administer every 4 to 6 hours if needed. (Consensus-Panel Expertise)
To reduce the risk of acute chest syndrome in adults and children hospitalized for a VOC,
Encourage use of incentive spirometry while awake. (Strong Recommendation, Moderate-Quality Evidence)
Encourage ambulation and activity as soon as possible.(Consensus-Panel Expertise)
In adults and children with VOC, use adjunctive nonpharmacologic approaches to treat pain such as local heat application and distraction. (Consensus-Adapted)
In euvolemic adults and children with SCD and a VOC who are unable to drink fluids, provide intravenous hydration at no more than maintenance rate to avoid overhydration. (Consensus-Adapted)
In adults and children with SCD and a VOC being treated with opioids, monitor for excessive sedation by measuring sedation with an objective measurement sedation scale and oxygenation levels. (Consensus-Panel Expertise)
Gradually titrated down parenteral opioids as VOC resolves. (Consensus-Panel Expertise)
In adults and children with SCD and a VOC, do not administer a blood transfusion unless there are other indications for transfusion (see the chapter “BloodTransfusion in the Management of Sickle Cell Disease” in these guidelines). (Moderate Recommendation, Low-Quality Evidence)
In adults and children with SCD and a VOC with an oxygen saturation <95 percent on room air, administer oxygen. (Consensus-Panel Expertise)
Exhibit 7. Acute Pain Algorithm